Hospital Housekeeping Outsourcing and Patient Safety Peer Reviewed
- Meeting report
- Open Admission
- Published:
Keeping hospitals make clean and safe without breaking the banking company; summary of the Healthcare Cleaning Forum 2018
Antimicrobial Resistance & Infection Control volume 7, Article number:132 (2018) Cite this article
Abstruse
Keeping hospitals make clean is a crucial patient safety outcome. The importance of the hospital surround in patient intendance has only recently been recognized widely in infection prevention and control (IPC). In order to create a movement for alter, a group of international infection control experts teamed upwardly with Interclean, the largest cleaning merchandise-show in the world to create the Healthcare Cleaning Forum. This newspaper is the result of this conference, which featured leaders in healthcare environmental scientific discipline from across Europe.
Although the available literature is limited, there is now enough show to demonstrate that maintaining the hygiene of the infirmary environment helps prevent infections. Still, expert interventional studies are rare, the quality of products and methods available is heterogeneous, and environmental hygiene personnel is often relatively untrained, unmotivated, nether-paid, and under-appreciated past other actors in the hospital. Coupled with understaffed ecology hygiene service departments, this creates lasting bug in regards to patient and healthcare worker safety.
The Healthcare Cleaning Forum was designed every bit a platform for healthcare experts, cleaning experts, hospital managers and industry to meet productively. The conference aimed to summarize the state-of-the-art knowledge in the field, create sensation and dialogue, challenge dogma and begin to shape a research agenda for developing the field of infirmary hygiene and environmental control. Hospital ecology hygiene is far more complex than other types of cleaning; further evidence-based inquiry in the field is needed. It involves the integration of electric current and new technologies with human being elements that must work together synergistically to reach optimal results. The pedagogy, training and career evolution, behavior, and work organisation of environmental hygiene personnel are at the core of the proposals for the cosmos of a global initiative. Ultimately, what is needed is a reevaluation of how hospitals view environmental hygiene: not just as an area from which to cut costs, but ane that can add together value. Hospitals and central stakeholders must work together to change how nosotros maintain the hospital environment in guild to better protect patients.
Introduction
Revolutions are oft started by ideas whose time take come. Compared to other domains in medicine, revolutions in the field of Infection Prevention and Control (IPC) are generally few and far between. The last ane was probably the global shift to using alcohol-based handrub (ABHR) instead of washing hands with soap and water, about 25 years ago- a seemingly small change in practice that continues to save millions of lives [ane,2,3]. Today, looking at the IPC mural, the 1 area that has been consistently undervalued and understudied is the role of the hospital environment in patient care. Keeping hospitals clean is not just an aesthetic, but a patient prophylactic issue.
Although the bachelor literature is limited, there is enough evidence to demonstrate that cleaning hospitals helps forbid infections. Still, expert intervention studies are rare, the quality of products and methods available is heterogeneous, and environmental hygiene personnel is often relatively untrained, unmotivated, under-paid, and under-appreciated by other actors in the hospital. Coupled with understaffed environmental hygiene services departments, this creates lasting issues in regards to patient and healthcare worker safety.
The situation is not helped past the lack of literature concerning the exact impact that a soiled or contaminated environment has on healthcare-associated infections (HAI). In social club to brainstorm the initiative to change how hospitals retrieve about their environment, a group of infection control experts teamed up with Interclean, the largest cleaning merchandise-show in the world, to create the Healthcare Cleaning Forum: a nexus where hospital managers, industry, and healthcare and cleaning experts could meet productively. For the kickoff time, Interclean dedicated an unabridged hall to cleaning in healthcare, and hosted a conference featuring leaders in healthcare environmental science from across Europe. The speakers summarized the state of the art noesis in the field, challenged the current dogma and began to shape a research calendar for developing the field of hospital hygiene and environmental control. This article outlines the major issues and points brought upward during the conference. It attempts to illustrate the large gap that exists betwixt environmental hygiene and the healthcare industry, also equally bring some much-deserved attention to a concept whose time has come.
Cleaning as a patient safety initiative
Nosotros demand to change how nosotros think most the hospital environs- if the risks of transmission are known, no ane wants to be the next patient in a contaminated room [four]. When the world inverse how they idea about paw hygiene 25 years ago [2, v, six], it realized how important hands were as the main vectors for spreading diseases from one patient to some other in hospital settings. It is estimated that over 50–70% of all HAI are spread through contaminated hands. Information technology is time to focus on the other 30–l%, a part of which might exist linked to environmental manual (Fig. 1). After all, "easily are really merely some other highly mobile surface in healthcare that are ordinarily contaminated and rarely disinfected" [vii]. Since there is a dynamic interchange between contamination on surfaces and hands [viii], some of the transfer in which contaminated easily are the final link include contaminated surfaces as links earlier in the chain of transmission. Ideally, infirmary environmental hygiene should follow the World Health Organization (WHO) model of "Clean Care is Safer Care" established for manus hygiene in 2005 [half-dozen], which spearheads good practices in more than than 180 countries today [ane, 9]. There is a need for creating evidence-based guidelines for infirmary cleaning, and for using those guidelines to develop the right tools for education and implementation.

"No i wants to stay in a contaminated room"
Although loftier-quality interventional studies are limited, at that place are plenty to bear witness that cleaning and disinfecting hospitals in order to prevent infection works. Analysis of numerous studies shows a clear correlation between "cleaning hygiene failures" and the number of intensive care unit-acquired infections (Fig. 2). Several studies showed that patients were much more likely to contract sure pathogens if the patient in the room before them was colonized or infected with a pathogen linked to HAI (Fig. iii) [4, 10,eleven,12]. There is a wealth of information on what products or chemicals eliminate which pathogens and how to utilise them. This includes efficacy and toxicity studies as well as a few clinical studies assessing the outcome of specific interventions to control outbreaks [x]. More inquiry is needed to mensurate the effects that cleaning methods have on HAI. Since improved environmental cleaning and decontamination measures are always bundled with other interventions during outbreaks, it is difficult to measure out their precise impact.
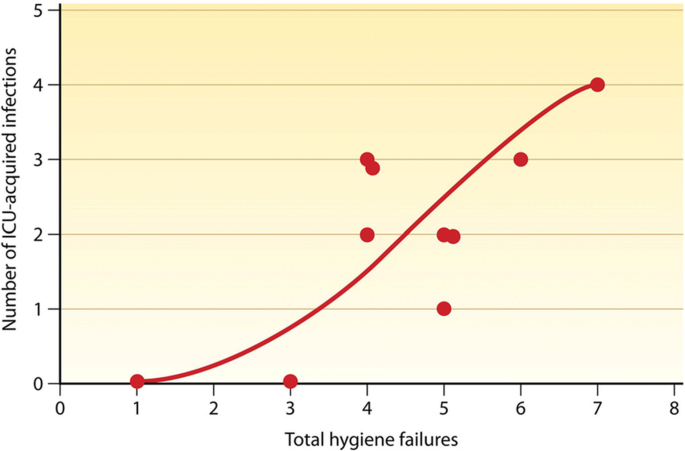
Human relationship between ecology bioburden and hospital-acquired infection [10]
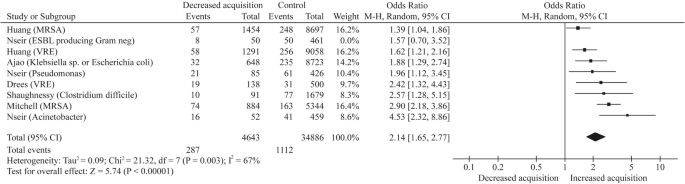
Risk of acquisition from prior room occupants past organism [four]. Risk of acquisition from prior room occupants by organism. M-H, Mantel–Haenszel; VRE, vancomycin-resistant enterococci; MRSA, meticillin-resistant Staphylococcus aureus; Ajao et al.'s study involved extended spectrum β-lactamase producing Klebsiella or Escherichia coli organisms. Acinetobacter: Acinetobacter baumannii; Pseudomonas: Pseudomonas aeruginosa. It was non possible to split up Klebsiella sp. and Escherichia coli data in the Ajao et al. report. Reprinted with permission from the Journal of Infirmary Infection
Cleaning in healthcare
Infirmary environmental hygiene is circuitous because it is dependent on the pathogen present and the product used to remove information technology. In that location are five main variables to cleaning, whether removing soil or disinfecting and cleaning on a microbiological level (Table 1; the acronym "Waste material" can be used to recall the v variables). These elements are: what production or intervention is applied, the technique and equipment used to apply the product, the type of surface, the level of contamination of the environment, and last but non least, the environmental hygiene personnel doing the cleaning [xiii]. If any one of these elements is defective, the cleaning will by definition be suboptimal. Because of this, irresolute cleaning practices in hospitals must be implemented through a multimodal strategy that takes these variables into account. The all-time cleaning substance in the world is useless if not applied correctly, and the best-trained personnel are useless if the product they are using is not effective against the particular pathogen that needs to exist removed or killed.
Merely what is "clean"? (Table 2) Maintaining a aseptic hospital environment is not simply almost removing soil, only too about organizing an environment that is optimal for patient safety. Obviously if an area is visibly dirty, one cannot disinfect information technology. Visibly soiled surfaces must kickoff be cleaned, and so, when or if appropriate, disinfected. Failure to practise so means that the infective organisms cannot exist targeted effectively [10]. The 2018 survey from the European network to promote infection prevention for patient condom (EUNETIPS) aimed to analyze how different hospitals evaluated and accept created their cleaning strategies [14]. Cleanliness of a hospital too plays a large role in patient perception of the healthcare setting, and consequently of patient satisfaction [xv, 16]. Patients are instrumental in convincing administrators to invest in cleaning, and must exist sensitized to the issues in order to be allies for creating change.
Available products
In improver to a vast array of detergents and cleaning/disinfecting equipment, common chemicals used for disinfection include: alcohol, chlorine and chlorine compounds, formaldehyde, glutaraldehyde, hydrogen peroxide, iodophors, ortho-phthalaldehyde, peracetic acid, phenolics, and fourth ammonium compounds [17]. This paper will not go into any particular on these products as such a discussion would be also extensive and was not the purpose of the Healthcare Cleaning Forum 2018.
An ideal product would exist effective against all bacteria, spores, viruses, and prions while having no impact on the environs and being completely safe also every bit easy to use. Currently no such production exists; thus choosing whatever product volition result in some level of tradeoff.
For example, hydrogen peroxide vapor does not get out whatsoever residues in the environment, just is expensive, can exist corrosive, and is difficult to use compared with liquid disinfectants. Chlorine solutions are effective against spores, just have a strong odor, go out residues, and may damage certain environmental surfaces. UV light leaves no residue but cannot disinfect areas that it cannot shine on straight. This is the case for every unmarried product available today; most only piece of work confronting certain types of pathogens, and others are toxic or degrade certain materials in the patient environment.
The human component
Just cleaning is not merely dependent on the chemicals used. The platonic environmental hygiene personnel (Table 2) would remain thorough and meticulous, and always use the correct technique, product and materials. Cleaning and disinfecting a hospital is a repetitive task that can quickly become mundane. Ecology hygiene personnel are often non trained sufficiently, and do non feel that they have the agency to brand a difference in patient safe. Additionally, the amount of work that they are expected to do is not ever in accordance with the fourth dimension assigned to the job. Inside the hospital hierarchy, environmental hygiene personnel are on one of the lowest rungs, and often credit is not given to them, especially considering the importance of their piece of work. In that location is a major problem with how "cleaners" are often perceived every bit menial and uneducated by the rest of the hospital staff. In many countries, particularly in loftier-resources settings, cleaning personnel frequently originate from outside of the country, and do not limited themselves in the local language, thus making discussions and interactive exchanges with other categories of wellness professionals hard or fifty-fifty impossible.
Additionally, few hospitals have sufficient systems in place to train and certify their cleaning staff. Without certification, advancement is unstructured and can be express since there is no way to gauge the quality of a staff as a whole. Oft there is a high turnover rate among personnel within the cleaning service or a language bulwark between the cleaners and the rest of the staff. Cleaning personnel must be trained to empathise why their work is important to the hospital, and need to be recognized and certified in order to improve motivation and compliance [18].
Logistics of hospital cleaning
The place of the environmental hygiene services department (Table two) within a infirmary is important, especially with regard to how they work together with the IPC service. Nursing assistants are generally responsible for cleaning ane part of the patient environment and the environmental hygiene personnel for another; merely oftentimes, respective tasks are not clearly defined. For case, if who needs to clean the bedside table is not explicitly stated, then in that location is a good adventure that that table may not be cleaned by anyone. In i survey, one third of environmental hygiene personnel admitted that they were not really clear well-nigh what they were responsible for [19]. Absences or shortage of staff on wards, and/or the transfer of responsibilities betwixt colleagues could complicate an already unclear state of affairs and result in crucial maintenance not being performed. This tin result in the spreading of disorder: a few minor mistakes, or disregard for a few of the rules, eventually crusade increased condone for rules in general amongst the whole staff [19].
In add-on to the aforementioned issues, environmental hygiene services are often outsourced to external companies. While probably non as much of an issue in a stairwell or an office, it is virtually impossible for a infirmary to optimize the cleaning staff and its quality if they accept little to no oversight of or influence on the environmental hygiene. Outsourcing is not necessarily bad, only the right atmospheric condition must be observed, and crucial areas need to be cleaned by trained and certified professionals, even if costs are bit higher initially.
Education, training and advice
So how can we effectively educate and train hospital personnel for modernistic environmental hygiene maintenance? While the scientific discipline of cleaning and disinfecting agents and equipment has evolved immensely in the last few decades, the education of cleaning personnel and their integration into healthcare worker teams has not. Cleaning and disinfecting hospitals is very different from cleaning public spaces such as hotels or offices; hospitals must realize this and adapt to the challenges. There is a range of environments within each hospital, from offices to intensive care units or hospital pharmacy services, some of which require specialized approaches to environmental hygiene maintenance. There are fifty-fifty different requirements for different sectors within the same department. The pathogens nowadays in hospitals can be quite different from those present in the community, and the patient population is more vulnerable. Each type of pathogen has its own specific transmission pattern, host affinity, and microbiological characteristics.
Leaders and trainers must be seen as legitimate by staff, and need to ensure their understanding and motivation. Only if at that place is a high process agreement in training tin can quality become routine; an informed person tends to be more compliant, and a compliant person is more motivated. Motivated teams are more than efficient and more aware, and individuals need to understand that anybody's work is important. Personal responsibleness and team cohesion require solid collaboration, which in turn requires the equality and realization of rights and duties. Repetition, feedback and squad-building assistance optimize functioning in environments that inherently foster human mistake. Analyzing hospital architecture, workflow, and ergonomics can get a long way to reducing information technology. It is important to realize that the best product, equipment or intervention is worthless without well-trained, responsible and compliant staff.
Possibilities of automation and self-disinfecting surfaces
Automation can exist useful, but currently does non replace the need for thorough manual cleaning. Although transmission cleaning and disinfection can exist qualitatively equally good equally motorcar automated disinfection (or even ameliorate in some instances), 1 has less oversight over humans, and they do not clean at their all-time all of the time. Ecology hygiene service managers can use a diverseness of tools including visual inspection, cultures, ATP meters or UV calorie-free reactive fluorescent markers to verify how well a given area has been cleaned and disinfected. Though even the best-trained people are prone to error, machines never skip any steps. Automated or semi-automatic room disinfection is not to replace personnel, but to raise the bar on the standard of disinfection and, in some instances, prevent work-related musculoskeletal constraints among environmental hygiene personnel. At some point, solely manual approaches are doomed to fail, as infirmary environments are intricate and difficult to maintain in an appropriately make clean state. In 1 study, upwards to 50% of an environs remained uncleaned later manual cleaning. Some other study showed that after four rounds of transmission cleaning and disinfection with a bleach solution, 25% of rooms were still contaminated with Acinetobacter baumanii [20]. Automated room disinfection with hydrogen peroxide vapor or ultraviolet light have shown promising results in targeting specific microorganisms, although they only piece of work once a room has already been manually cleaned to remove soil [21].
Beyond machines, at that place is an of import need for more research into surfaces that inherently inhibit bacterial contamination or that have self-disinfecting backdrop. A few that accept been studied are the micro-patterning of surfaces or the inclusion of copper in them in society to reduce contagion [11]. The thought of having something permanently in the patient environs that is always working is an bonny one (although perhaps expensive): if one can control the level of contamination at the source, then there is less to remove and less hazard for sub-optimal cleaning and disinfection. Further research, including unbiased, loftier-quality clinical efficacy and effectiveness studies are all the same still needed earlier further recommendations tin can be made regarding these materials [22, 23].
Toll vs. value of hospital cleaning and disinfection
Information technology is imperative to develop a new and efficient model for hospital environmental hygiene maintenance. The render on investment for successful hand hygiene promotion has been shown to up to 23 times the initial amount invested [24,25,26]. In social club to have like figures for hospital environmental hygiene, we need to showtime empathize what the price of maintaining a clean infirmary environment is, and what its value is. Although many hospitals are quick to spend money on new software, specialized staff and fancy equipment, they often await at maintaining the environment hygiene as an opportunity to relieve in the budget.
Hospitals ofttimes try to cut ecology hygiene maintenance costs as much equally possible, both in the products that they use, and in the training and continued education of their workforce. The essential shift in approach needs to happen in how hospitals assess this cost and value. Considering the costs of not cleaning can affect numerous budgets inside a infirmary, information technology is hard to accurately account for them. Hospitals need to look beyond actual expenditures to averted expenditures, such as increase in patient-days due to HAI, besides every bit opportunity costs such as hospital staff fourth dimension or missed surgical acquirement due to increased turnaround fourth dimension in an operating theater. There are also increases in costs associated with antimicrobial resistance in HAI, which has a cost estimated at over €85 trillion ($100 trillion) globally past 2050 [27]. For case, 1 relatively small outbreak with approximately 40 cases cost a hospital over €ane meg [28]. Prevention is ever better and less expensive than a cure, especially when we are running out of antibiotics. So when making a decision near which environmental hygiene maintenance systems to buy, which products to use, or how much to invest in training the cleaning personnel, hospitals would exercise well to look at the costs of not doing so, or deciding on a cheaper solution. In order to salvage money in the long-term and improve patient satisfaction, hospitals need to invest in quality beyond the board whether in materials, disinfectants, technological innovation, or the training, educational activity, and certification of their workforce (Fig. 4).

Hospitals should value environmental hygiene cleaning and maintenance
A time for cooperation
It is imperative to develop public-private partnerships in the field of clean hospitals. Industry and academia both have a role to play in raising standards and providing hospitals with the all-time possible products and methods. First, currently marketed sub-standards products and methods should be suppressed. Ultimately, the difference volition no longer be betwixt good and bad products on the market, simply within implementation and training of those products and technologies.
Cleaning and ecology maintenance is a science. Initially, assessing the approach for the hygiene of a toilet seat seems almost redundant. However, many of the questions around this seemingly simple activity require written report and scientific assessment. One must make up one's mind material to use to clean the toilet seat (e.g. microfiber or cotton fiber textile), which liquid agent to use (eastward.m. a detergent or a disinfectant and, if a disinfectant, which one), and the ideal frequency of the cleaning and disinfection (e.g. daily, after each use, or both). Many questions remain unanswered; some are addressed in the Appendix (see Appendix). Hospitals must become out of the roughshod circle of cutting costs and instead assess value. They must realize that being a hospital "cleaner" is not a job simply a profession, and invest in their workforce. Academics must encourage further studies (run across research agenda, Tabular array 3) as well as weave together the data available in order to present hospitals with a disarming business case of why to invest in infirmary cleaning.
Considering make clean hospitals is an idea whose fourth dimension is now.
Annotate
The authors alone are responsible for the views expressed in this article and they practice not necessarily stand for the views, decisions or policies of the institutions with which they are affiliated.
Abbreviations
- ABHR:
-
Alcohol-based handrub
- HAI:
-
Healthcare-associated infection
- IPC:
-
Infection prevention and command
- WHO:
-
Earth Health Organisation
References
-
Earth Wellness Organisation. WHO Guidelines on Manus Hygiene in Health Intendance. 2009.
-
Vermeil T, et al. Manus hygiene in hospitals: beefcake of a revolution. J Hosp Infect. 2018.
-
Grayson ML, et al. Furnishings of the Australian National Hand Hygiene Initiative after 8 years on infection control practices, health-care worker education, and clinical outcomes: a longitudinal study. Lancet Infect Dis. 2018;0.
-
Mitchell BG, Dancer SJ, Anderson M, Dehn E. Risk of organism acquisition from prior room occupants: a systematic review and meta-assay. J Hosp Infect. 2015;91:211–7.
-
Pittet D, et al. Effectiveness of a infirmary-broad program to better compliance with hand hygiene. Infection Control Programme. Lancet Lond Engl. 2000;356:1307–12.
-
Pittet D, Donaldson Fifty. Clean care is safer care: a worldwide priority. Lancet Lond Engl. 2005;366:1246–vii.
-
Otter J. The countdown healthcare cleaning forum. Reflect Infect Prevent Contr. 2018.
-
Pittet D, et al. Evidence-based model for hand transmission during patient care and the part of improved practices. Lancet Infect Dis. 2006;6:641–52.
-
Kilpatrick C, Storr J, Allegranzi B. 'A Worldwide WHO Hand Hygiene in Healthcare Campaign' Ch. 38 in Hand Hygiene: A Handbook for Medical Professionals. Hoboken: Wiley-Blackwell; 2017. pp. 275–284.
-
Dancer SJ. Controlling hospital-acquired infection: focus on the function of the environment and new Technologies for Decontamination. Clin Microbiol Rev. 2014;27:665–90.
-
Weber DJ, Rutala WA, Miller MB, Huslage K, Sickbert-Bennett E. Part of hospital surfaces in the manual of emerging wellness care-associated pathogens: norovirus, Clostridium difficile, and Acinetobacter species. Am J Infect Command. 2010;38:S25–33.
-
Otter JA, Yezli S, Salkeld JAG, French GL. Bear witness that contaminated surfaces contribute to the transmission of infirmary pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am J Infect Control. 2013;41:S6–S11.
-
Albrecht, P. HUG Entretien environment du patient. 2018.
-
Parneix, P. Cleaning as a patient safety initiative. 2018.
-
Quintana JM, et al. Predictors of patient satisfaction with hospital wellness care. BMC Health Serv Res. 2006;half-dozen:102.
-
Schoenfelder T, Klewer J, Kugler J. Determinants of patient satisfaction: a study amongst 39 hospitals in an in-patient setting in Germany. Int J Qual Health Care. 2011;23:503–9.
-
Mitchell BG, et al. Changes in knowledge and attitudes of hospital environmental services staff: the researching effective approaches to cleaning in hospitals (REACH) report. Am J Infect Control. 2018;46(9):980–5.
-
Voss, A. Cleaning in healthcare: the new concept. 2018.
-
Strassle P, et al. The effect of terminal cleaning on environmental contamination rates of multidrug-resistant Acinetobacter baumannii. Am J Infect Command. 2012;twoscore:1005–7.
-
Havill NL, Moore BA, Boyce JM. Comparison of the microbiological efficacy of hydrogen peroxide vapor and ultraviolet lite processes for room decontamination. Infect Control Hosp Epidemiol. 2012;33:507–12.
-
Mann EE, et al. Surface micropattern limits bacterial contagion. Antimicrob Resist Infect Control. 2014;iii:28.
-
Hall L, et al. Researching effective approaches to cleaning in hospitals: protocol of the REACH study, a multi-site stepped-wedge randomised trial. Implement Sci. 2016;11:44.
-
M Abbas et al. Conflicts of interest in infection prevention and control research: no smoke without burn. A narrative review. Intensive Care Med Press; 2108.
-
Pittet D, Sax H, Hugonnet S, Harbarth S. Cost implications of successful hand hygiene promotion. Infect Control Hosp Epidemiol. 2004;25:264–6.
-
Graves North. The economic impact of improved hand hygiene. In: Hand Hygiene: Wiley-Blackwell; 2017. p. 285–93. https://doi.org/10.1002/9781118846810.ch39.
-
Craig, D, et al. Economical evaluations of interventions to prevent healthcare-associated infections literature review. 2017.
-
The Review on Antimicrobial Resistance Chaired by Jim O'Neill. Tackling Drug Resistant Infections Globally: Concluding Study and Recommendations. 2016.
-
Otter JA, et al. Counting the price of an outbreak of carbapenemase-producing Enterobacteriaceae: an economical evaluation from a hospital perspective. Clin Microbiol Infect. 2017;23:188–96.
-
Disinfection and Decontamination: Principles, Applications and Related Issues Edited past Gurusamy Manivannan Boca Raton, FL: CRC Press, 2007. 512 pp., Illustrated.
-
Detergent | Definition of detergent in English past Oxford Dictionaries. Bachelor at: https://en.oxforddictionaries.com/definition/detergent. Accessed xvi Aug 2018.
-
Disinfectant | definition of disinfectant past Medical dictionary. Available at: https://medical-lexicon.thefreedictionary.com/disinfectant. Accessed 16 Aug 2018.
-
Disinfectant | Definition of Disinfectant by Merriam-Webster. Available at: https://world wide web.merriam-webster.com/dictionary/disinfectant. Accessed: 16 Aug 2018.
-
Fumigate | Definition of Fumigate by Merriam-Webster. Available at: https://www.merriam-webster.com/dictionary/fumigate. Accessed 16 Aug 2018.
-
Healthcare forum. Available at: https://world wide web.intercleanshow.com/en/amsterdam/healthcare-cleaning-forum. Accessed 26 June 2018.
-
WHO. WHO guidelines on manus hygiene in health intendance. WHO. Available at: http://www.who.int/gpsc/5may/tools/9789241597906/en/. Accessed 26 June 2018.
-
Allegranzi B, et al. Brunt of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet Lond Engl. 2011;377:228–41.
-
Allegranzi B, et al. Global implementation of WHO'southward multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis. 2013;13:843–51.
-
Pittet D. Mitt hygiene: It's all nigh when and how. Infect Control Hosp Epidemiol. 2008;29:957–9.
Acknowledgements
The authors would like to give thanks Interclean, CAP Partners and colleagues and collaborators who made the Healthcare Cleaning Forum possible, especially Marianne Kemmer, Sofie Struve Løgstrup, Henrik J. Nielsen, Paul Riemens, and Rob den Hertog. They also wish to thank Markus Dettenkofer for his contribution. The authors would also like to accost their special thanks to Nasim Lotfinejad from the Department of Inquiry, Faculty of Medicine, Mashhad Academy of Medical Sciences, Mashhad, Iran, for her illustrations.
Funding
Principal funding past the Infection Control Program & WHO Collaborating Eye on Patient Safety (SPCI/WCC), University of Geneva Hospitals and Faculty of Medicine, Geneva, Switzerland; hand hygiene inquiry activities at the SPCI/WCC are supported by the Swiss National Science Foundation (32003B_163262).
Andreas Voss has received grants past the Framework Programme of the European Commission, Interreg, ZonMW, and VWS. In add-on he received funding or speakers fees by Ophardt, Deb, Ecolab, Momentum Bioscience, Brill & Partner, Gama, bioMerieux, UVDI, and 3M.
Didier Pittet has received funding by the European Commission and the Swiss National Science Foundation for several research and clinical studies; he as well works with the WHO in the context of the WHO initiative Private Organizations for Patient Prophylactic (POPS) Paw Hygiene. The aim of this WHO initiative is to harness industry strengths to align and better implementation of WHO recommendations for manus hygiene in healthcare in different parts of the world, including in to the lowest degree developed countries. In this instance companies/manufacture with a focus on manus hygiene and infection control related advancement accept the specific aims of improving access to affordable manus hygiene products likewise as supporting pedagogy and research.
The 2018 Healthcare Cleaning Forum was logistically supported by Interclean and benefitted from the coordination efforts of CAP Partners.
Availability of data and materials
Information sharing non applicable to this article equally no datasets were generated or analyzed during the current written report.
Author information
Affiliations
Contributions
All authors read and canonical the terminal manuscript. AP drafted the manuscript, all authors edited and approved it. Content was generated from the all authors. All authors except for AP spoke at the conference.
Respective writer
Ethics declarations
Ethics approval and consent to participate
Delight run across signed author forms, upstanding blessing was not needed for this newspaper.
Consent for publication
Not applicable
Competing interests
Alexandra Peters and Didier Pittet accept no conflicts of interest to declare and have received funding from the Swiss National Science Foundation for inquiry.
Andreea Moldovan: has no conflicts of interest to declare and has received funding from St. Constantin Hospital, Brasov, Romania.
Jon Otter has, in the last 3 years, received Academic fees from CAP Partner, Centre for Clinical Infection and Diagnostics Inquiry, Elsevier, and IDSA; consulting fees from Aquarius, Arthur D Little, Fields Consulting, Gama Healthcare Ltd., GK Intelligence Limited, Pfizer Ltd.; and speaker fees from 3M, Hospital Da Luz, Portugal, Odense University Hospital (Denmark), Drape Medical Ltd., Serosep Ltd., Society for Applied Microbiology, Virox, and Webber Training.
Pierre Parneix French Ministry building of Wellness through the Regional Health Agency of Nouvelle Aquitaine.
Publisher's Notation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
During the speaker presentations at the Healthcare Cleaning Forum conference in Amsterdam (May 16th, 2018), audition participants were able to ask questions directly via their smartphones. A total of 87 questions were submitted. Some of these questions were chosen and so posted on the screen in a higher place the speakers, who and so addressed them directly after each presentation. These questions, likewise as some that in that location were not posted during the conference, have been organized, and in some cases, combined or rephrased for clarity. The responses from the speakers accept been synthesized in the table below.
Questions answered directly in the paper are not listed in the Table.
Rights and permissions
Open Access This article is distributed nether the terms of the Creative Eatables Attribution four.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted employ, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(southward) and the source, provide a link to the Creative Commons license, and signal if changes were fabricated. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/cypher/one.0/) applies to the information made available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Cite this commodity
Peters, A., Otter, J., Moldovan, A. et al. Keeping hospitals clean and rubber without breaking the bank; summary of the Healthcare Cleaning Forum 2018. Antimicrob Resist Infect Control 7, 132 (2018). https://doi.org/10.1186/s13756-018-0420-3
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1186/s13756-018-0420-3
Keywords
- Infection prevention
- Cleaning
- Disinfection
- Environment
- Healthcare-associated infection
- Public health
- Environmental hygiene
- Hand hygiene
- Infection control
- Antimicrobial resistance
Source: https://aricjournal.biomedcentral.com/articles/10.1186/s13756-018-0420-3
0 Response to "Hospital Housekeeping Outsourcing and Patient Safety Peer Reviewed"
Post a Comment